
Cystic Fibrosis Centre
Our mission is to drive therapy discovery and the clinical application of new therapies, care, and education for cystic fibrosis (CF) that benefit children and youth around the world. We envision new technologies in large scale genomics, and therapy validation in patient-derived tissues, will impact transformational changes in CF patient health by enabling personalized therapies.
Together, our team of researchers and clinicians have provided a comprehensive understanding of the disease and helped move new CF therapies into the clinic.

Treating cystic fibrosis in children
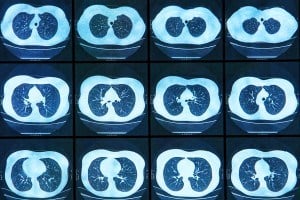
Cystic fibrosis (CF) affects multiple organs and can cause gastrointestinal disease, liver disease, pancreatic disease, reproductive disorders and diabetes. CF can also lead to lung disease, the most common cause of lower life expectancy related to CF.
The CF Centre’s research approach spans the full spectrum, from detailed studies of the underlying genetic defect, its molecular structure, and function to patient-based research and excellent clinical care. This multidisciplinary approach has characterized CF research at SickKids for decades, from first recognizing the need for high-calorie diets to maintaining CF patient health (Corey and Crozier, 1976) to the discovery of the CF gene (Riordan, Rommens and Tsui, 1989).
State-of-the-art laboratory research in CF is linked to outstanding clinical research and clinical care in a rich collaborative environment that has existed within SickKids for the past three decades. The clinical program for CF at SickKids is known as one of the leading care facilities in the world and has a well-established reputation for its excellence in multidisciplinary care.

The CF Mutation Database
Since 1989, SickKids has fostered and maintained a comprehensive website, with details on over 1600 mutations in the CF gene that cause CF and related diseases. With contributors and users from around the world, the CF Mutation Database is a major resource for clinical and basic research and serves as a model for other genetic disease databases.

The Program for Individualized CF Therapy (CFIT)
In 2015, SickKids partnered with Cystic Fibrosis Canada and launched the Program for Individualized CF Therapy (CFIT). The CFIT Program is developing tools and technologies for personal medicine in CF. Visit the CFIT website for the latest advances and information for researchers and patients.
Cystic Fibrosis Centre Leadership

Medical Director
Program Head and Senior Scientist, Translational Medicine Paediatric Respirologist, Division of Respiratory Medicine


Executive Council
Pediatric Gastroenterologist/Pancreatologist, Division of Gastroenterology, Hepatology and Nutrition Associated Senior Scientist, Translational Medicine


Executive Council
Pediatric Respirologist, Division of Respiratory Medicine Director, Cystic Fibrosis Clinic Medical Director, Lung Transplant Program


Program Coordinator

Ratjen Lab
The Ratjen lab focusses on ways to improve the lives of people with CF by performing clinical trials of new therapies including medications that treat the underlying defect in CF. A special focus is also on finding better methods to monitor CF lung disease which can be used to assess clinical status and treatment response. We are linked with centres in Canada, the US, Europe and Australia and work together closely to advance CF care.

Bear Lab
The Bear Lab applies advanced technologies to study stem cells and fresh tissues donated by people with Cystic Fibrosis caused by a diverse range of mutations in the CFTR gene. These cell and tissue donations are maintained in the CFIT Bioresource at SickKids and available to all CF researchers. With these studies, we are developing personalized, molecular signatures for CF disease progression and the impact of therapies. In the future, we will apply these tools to advance the development of precision genetic medicines for people with CF caused by rare mutations who lack effective therapies.

Gonska Lab
The Gonska lab and clinical research team studies CFTR function and response to CFTR modulators in human cells (nasal, bronchial, intestinal) from people with CF and CFTR-related disorder, and interrogates clinical markers that predict the risk for CF/CFTR-related organ disease.

Hu Lab
The Hu lab has expertise in engineering viral vectors for gene editing and gene replacement therapy, and in delivering genes to airways of small and large animal models.

Moraes Lab
The Moraes lab has expertise in growing airway cells obtained from human donors (nasal, bronchial). These human cells can be used to test drugs for CFTR functional rescue, to develop new approaches to rescue CFTR function and to learn more about CFTR biology.

Waters Lab
The Waters lab studies CF bacterial biofilms and polymicrobial interactions and conducts translational studies in CF airway infections.

Wong Lab
The Wong lab has expertise in stem cell biology and develops induced pluripotent stem cell (iPSC)-based lung models for disease modeling and therapy discovery.

